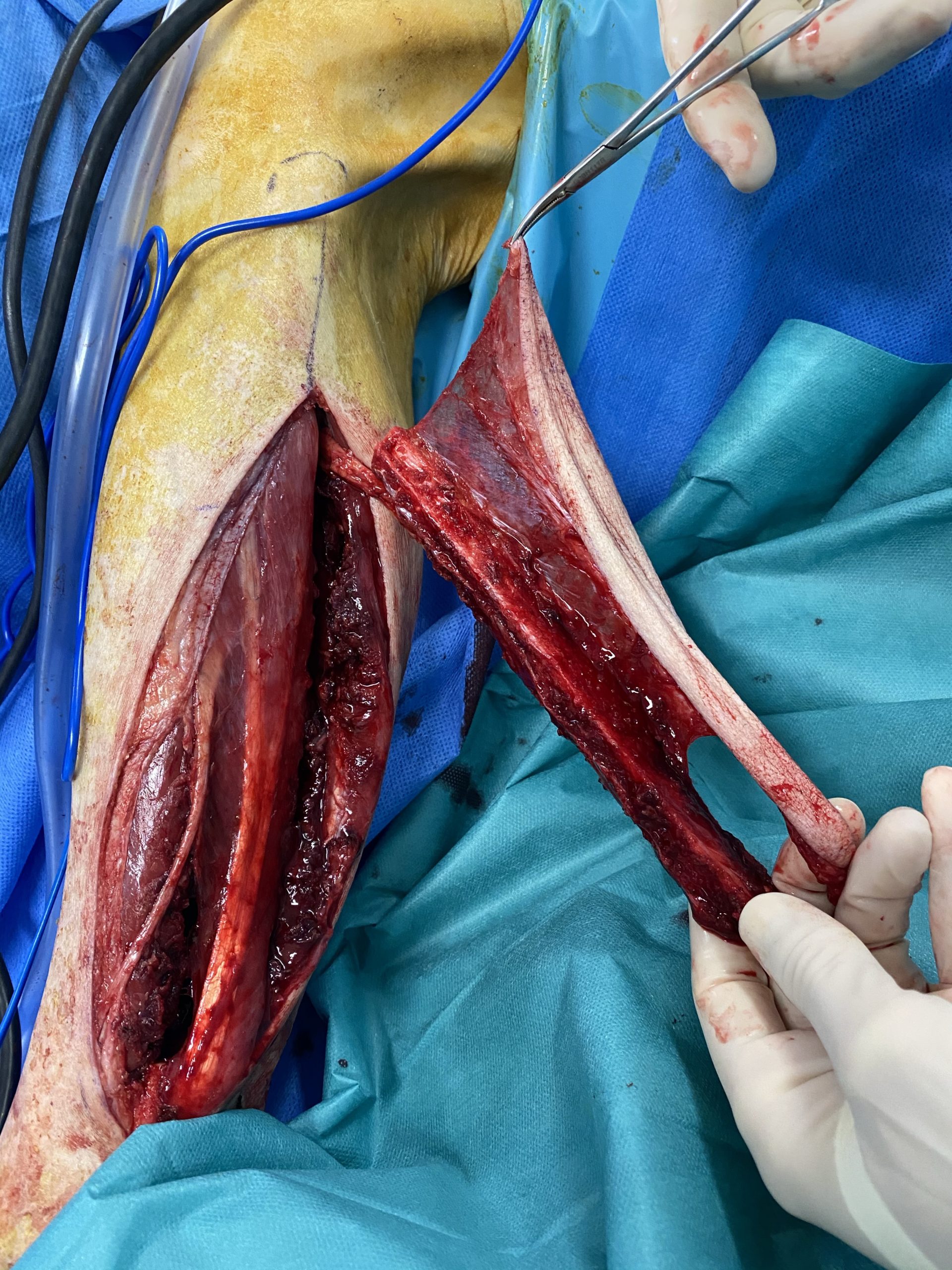
In my department we do around 40-50 free flap surgeries for ENT cancer per year. Here is the usual process
- we often but no always do the endoscopy for the diagnostic
- we often perform a gastrostomy before the major surgery
- the patient is seen by a nurse who explains the process during the hospitalization and thee major challenges for the patient
- so do we as anesthetists during our consultation prior to the surgery
- Since I can do basic echocardiography, I do it by myself when I have a doubt
- I am not a great believer in iron injections but we check the ferritin and transferrin saturation coefficient prior to the surgery
- The day before and the day of the surgery the patient is given gabapentine 600 mg
- antibiotics : amox/clavulanate for 48h
- common anesthesia protocol is
- remifentanil
- I prefer propofol over desflurane for the planet and for oncologic concerns bur the level of proof is rather low
- IV lidocaine
- ketamine infusion
- dexamethasone (might be good against cancer ?)
- regional anesthesia of the limb which gives the flap (sometimes a catheter stays in place, in this case we put it the day before the surgery)
- we put an artery catheter to monitor the arterial pressure
- I always put a BIS or Entropy monitoring device. We do not have NIRS devices.
- a tracheostomy is performed in 99% of cases (we mostly do oropharyngectomies)
- venous intermittent mechanical compression
- we try to avoid central venous catheterism
- aspirin and 50 ui/kg of heparin is given for the free flap. No rinsing of the vessels, no vasodilatators, no magic bullet. I have ideas for free flap optimization but nothing has proved to be great according to this answer from Pr Lantieri
Est-ce que vous avez une expérience de sauvetage des lambeaux libres avec des dérivés nitrés ? Merci #DocTocToc Do you have any experience of free flap salvage with nitrates/nitro drugs ? Thanks #anesthesia #surgery #ENT
— nfkb (@nfkb) July 23, 2019
-
- we use a lot of noradrenaline/norepinephrine to optimize hemodynamics. I cannot remember precisely on the top of my head but when I was working in the GI surgery departement there was a publication that giving noradrenaline to maintain a MAP of 65 mmhg was better for thee gastroplasty than the alleged concerns of a « bad vasoconstriction »
- I personaly only use Ringer Lactate for fluid maintenance and i give red blood cell when the patients is obviously bleeding, I like the idea that fresh frozen plasma might be good for thee endothelium but there is no proof at all for this idea besides real hemorragic shock (Dr Jakob Stensballes’ work). I try to have a balance between restrictive and liberal fluid maintenance. I avoid too quick fluid boluses to avoid small capillaries damage. I like to be around 5 ml/kg/h of RL. Other colleaguees give macromolecules, expecially albumin. I very seldom do this (almost no macromolecules)
- We are more and more prone to do tranexamic acid. But I don’t know exactly why I am biaisd against it but I am. I am still afraid of the theombo-embolic risk. Maybee it’s stupid… I need to search the litterature on the subject of strategies to avoid transfusions in canceer surgery (we do not do EPO)
- morphine, paracetamol and ketoprofene are given at the end of the surgery
- despite good surgeons, these patients often receive transfusions, especially on Day 2 to 5